AITA for refusing to switch hospital rooms when my sister said my crying baby was “triggering her”?
Oh, the joys and challenges of welcoming a new baby! It's a time filled with overwhelming love, profound exhaustion, and often, unexpected family drama. Navigating the postpartum period is already a monumental task, requiring every ounce of a new parent's strength and focus. But what happens when a family member's personal struggles clash directly with the raw, undeniable needs of a newborn?
Today, we're diving into a story that brings this very conflict to the forefront. Our OP, a brand-new mother, found herself in a deeply uncomfortable position when her sister, also a hospital patient, made a truly shocking request. It’s a tale that pits maternal instincts against claims of personal triggers, all within the sterile, unforgiving environment of a hospital. Let's get into it.

"AITA for refusing to switch hospital rooms when my sister said my crying baby was “triggering her”?"
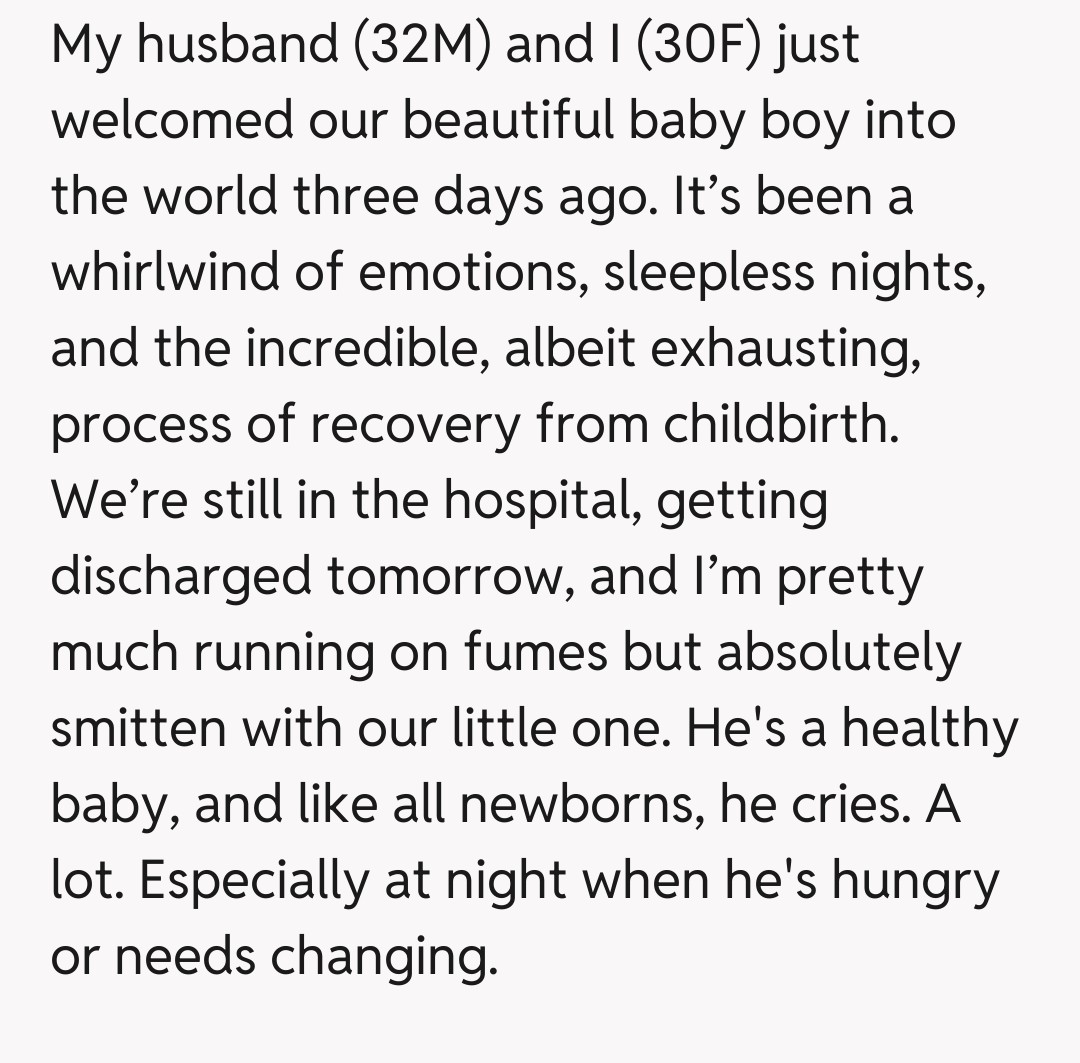

This scenario highlights a really tough situation where legitimate needs clash, and it's easy for emotions to run high. On one hand, we have a new mother recovering from childbirth, dealing with the natural chaos of a newborn, whose primary focus must be on her baby's well-being and her own recovery. The postpartum ward is specifically designed for mothers and infants, and a baby's cries are an expected, inherent part of that environment.
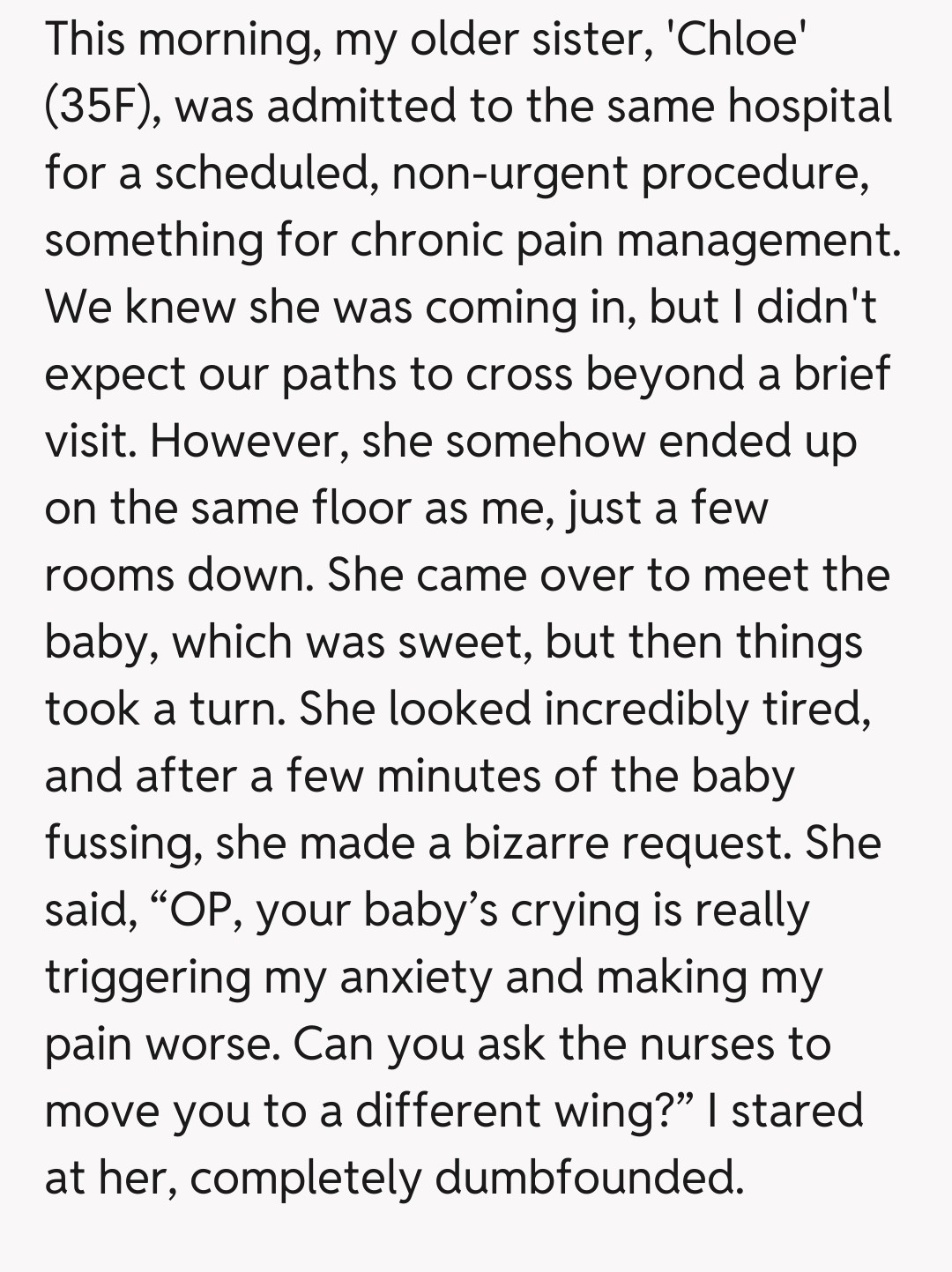
Then we have the sister, who is also a patient, dealing with chronic pain and anxiety. Her feelings of being triggered are likely very real and distressing for her. Hospitals, while places of healing, can be incredibly stressful and overstimulating environments for anyone, let alone someone with heightened sensitivities. Her request, while seemingly unreasonable to OP, likely stemmed from genuine discomfort.
However, the practicality of the situation leans heavily towards OP. A hospital's postpartum unit is not a quiet recovery ward for other patients. Moving a new mother and her infant, disrupting feeding schedules, sleep, and medical monitoring, is not a simple request. The hospital’s structure and priorities would almost certainly place the mother-baby unit’s stability above accommodating a non-postpartum patient’s preference for quiet.
Ultimately, while empathy for the sister’s pain and anxiety is warranted, expecting a newborn to be silent or a new mother to uproot her entire recovery setup is simply not feasible or fair. The sister's responsibility is to communicate her needs to the hospital staff who can explore solutions appropriate for her situation, rather than placing the burden on a vulnerable new mother.
The Internet Weighs In: Is Family Obligation Stronger Than Postpartum Peace?
The comments section on this one exploded, and it’s clear where the vast majority of opinions landed. Readers overwhelmingly sided with OP, emphasizing the unique and non-negotiable needs of a new mother and her baby. Many pointed out the inherent absurdity of expecting a newborn to be silent or for a postpartum unit to be quiet, highlighting a significant lack of understanding from the sister.
There was a strong current of support for maternal rights and the idea that a hospital’s postpartum wing is precisely for this kind of 'noise.' While some acknowledged the sister’s pain, they firmly stated it was the hospital’s responsibility to manage her triggers, not the new mother's. The consensus was clear: OP's refusal was not just reasonable, but entirely necessary.


This situation is a stark reminder of the intense vulnerability of the postpartum period and the sometimes-unreasonable expectations placed upon new mothers. While family dynamics are complex, the needs of a newborn and a recovering parent must take precedence. It's crucial for family members to offer support and understanding during such a delicate time, rather than add to the immense pressures. Hopefully, this story serves as a reminder for all of us to extend grace and practicality, especially in emotionally charged environments like a hospital.